What is a glioblastoma?
Glioblastoma (GBM) is a type of malignant tumor that invades and destroys our brain tissue in a quick and aggressive manner [1]. It is often referred to as a grade IV astrocytoma or “primary” brain tumor [1]. However, GBMs can also be classified as de novo, meaning they form without a pre-existing lower-grade glioma, or secondary, which is when a low-grade tumor develops into the GBM [2]. The tumor forms in the brain or spinal cord so it generally does not spread to other parts of the body as opposed to “secondary tumors,” which are tumors traveling from other body parts to the brain [1]. Unfortunately, glioblastoma is quite deadly, especially as treatments are not perfected yet [1]. In fact, only 40% survive the first year following diagnosis and 17% for the second year [3]. Despite this, glioblastoma is the most common malignant tumor and often appears at the age of 64 in men or Caucasians [2]. While symptoms depend on the area of your brain affected, patients may experience persistent headaches, disturbed vision, vomiting, memory loss, and several other impaired bodily processes [3].
What is the role of gene mutations?
The Cancer Genome Atlas (TGCA) project identified three key signaling pathways (the tumor protein p53 pathway, the receptor tyrosine kinase signaling pathway, and the retinoblastoma pathway) that are involved in or act as a disruptor to cell growth and tumor development [4]. GBMs have a modification in these pathways that leads to uncontrolled cell growth and increased cell survival, such as being able to bypass checkpoints in the cell cycle or avoid apoptosis [4]. Alterations to the epidermal growth factor receptor (EGFR) are commonly associated with primary GBMs [4]. More specifically, the overexpression and amplification of the EGFR gene [4]. EGFRvIII is the most typical EGFR mutant, produced by the deletion of exons (regions that can code protein) 2 to 7 from the EGFR gene [4]. EGFR gene amplification is strongly associated with EGFR protein overexpression, and only 10% of GBMs overexpress EGFR without gene amplification [4]. A study also proves this as EGFRvIII is found in 41% of GBMs with EGFR amplification but only appears in 5% of GBMs that do not have accompanying EGFR gene amplification, which suggests EGFR gene amplification may take place before EGFRvIII mutation [4]. EGFR gene amplification and overexpression are frequently seen in small-cell GBMs but rarely appear in gliosarcomas or giant-cell GBMs [4]. Additionally, a study showed that 74% of GBMs with strong EGFR protein expression demonstrated diffuse EGFR gene amplification (meaning it spreads across the tumor cells) and 16% exhibited focal EGFR gene amplification [4]. However, GBMs with no EGFR protein expression revealed no diffuse gene amplification and 7% focal gene amplification [4].
TP53 is another major dysregulated gene in cancers that encodes the P53 protein [5]. P53 maintains cellular homeostasis, controlling cell multiplication, survival, and genome integrity [5]. It also regulates gene transcription (the making of an RNA copy from the DNA sequence) and has been shown to be associated with cellular metabolism, invasion, immunity, and more [5]. The Cancer Genome Atlas GBM project showed that around 85% of tumors had a deregulated P53 pathway and approximately 28% had a mutated TP53 gene [5]. For further context, P53 is able to change the expression of several genes involved in the cell cycle, allowing it to suppress tumor activity [5]. P53 is activated when we see things like DNA damage, anomalous growth signals, and other signs [5]. TP53 mutations drive tumor formation in GBM but other genes like PTEN are also mutated in order to develop GBM [5]. However, TP53 and PTEN genes have not been proven to have prognostic significance yet [6].
Furthermore, over 70% of cases found IDH1 mutations in secondary glioblastoma and low-grade gliomas [6]. IDH1 and IDH2 genes typically convert isocitrate to alpha-ketoglutarate [7]. However, mutations in these genes lead to the conversion of alpha-ketoglutarate into 2-hydroxyglutarate, which promotes the development of gliomas [7]. A case study also concluded that oncogenesis may depend on the IDH mutation status [7]. This is shown by how the IDH1-mutant cells struggle with reductive carboxylation under hypoxia and depend on oxidative metabolism, whereas IDH2-mutant cells can maintain reductive carboxylation under hypoxia [7]. IDH1 and IDH2 mutations that occur at the same time are also extremely rare, where a TCGA database analysis of lower-grade gliomas and glioblastoma only identified two instances of concurrent IDH1 and IDH2 mutation out of 794 cases [7].
Diagnosis & Treatments
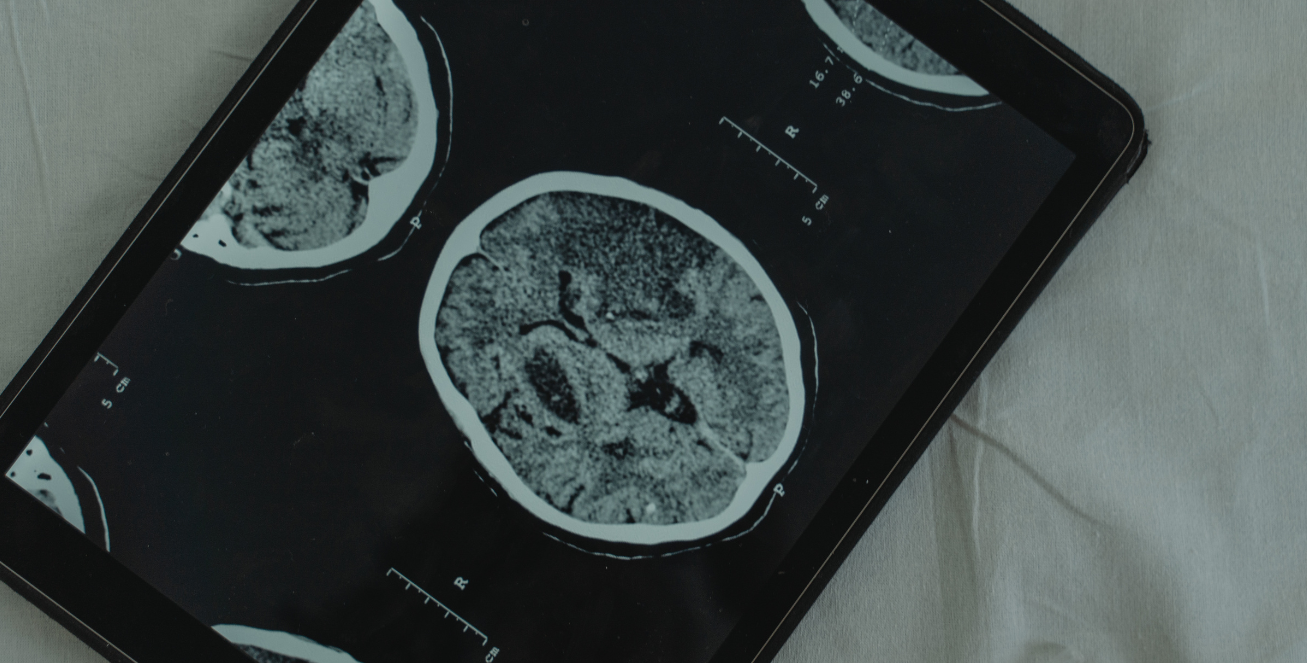
These gene mutations present an optimistic way to identify and diagnose glioblastoma and other cancers. Neuroimaging and physical exams are also common methods of GBM diagnosis, where doctors utilize computed tomography (CT) or magnetic resonance imaging (MRI) scans to identify tumor formation and follow up with a biopsy to confirm the diagnosis [8]. When it comes to treatment plans, surgical resections are generally done, where the affected tissue is surgically removed [8]. It’s also often followed by radiochemotherapy, which is standard in the treatment of many other types of cancers [8]. Moreover, some types of genetic mutations play a role in the resistance to GBM treatments. For example, the overexpression of EGFR and the EGFRvIII mutation increases the aggressiveness and invasion of the tumor, making it more resistant to targeted therapies [9]. Another example is the MGMT gene, an endogenous DNA repair enzyme, which counters the TMZ treatment, a type of chemotherapy drug [10]. MGMT is able to remove the methyl group in O6-methylguanine and repair the damage caused by the drug, reducing the effectiveness of TMZ treatment in GBM [10].
What’s Next?
Overall, GBM still stands as one of the most difficult and challenging cancers to treat with its aggressive nature and constant low survival rates. There is much research to be done on advancing current technology to better treat GBM and other gliomas. One specific opportunity would be looking into therapies that target specific mutations associated with GBM – as I have detailed above – or understanding how we can mitigate the effects of gene mutations against treatment resistance. Even more, incorporating artificial intelligence and machine learning into analyzing GBM may also offer some worthwhile findings.
Works Cited
- Glioblastoma Research Organization. (n.d.). Glioblastoma Symptoms: How to Spot the Signs of This Deadly Brain Cancer Tumor. Glioblastoma Research Organization. https://www.gbmresearch.org/blog/symptoms-of-brain-cancer-tumor
- Davis M. E. (2016). Glioblastoma: Overview of Disease and Treatment. Clinical journal of oncology nursing, 20(5 Suppl), S2–S8. https://doi.org/10.1188/16.CJON.S1.2-8
- Thakkar, J. P., Peruzzi, P. P., & Prabhu, V. C. (2024, April 15). Glioblastoma Multiforme. AANS. https://www.aans.org/patients/conditions-treatments/glioblastoma-multiforme/
- Hatanpaa, K. J., Burma, S., Zhao, D., & Habib, A. A. (2010). Epidermal growth factor receptor in glioma: signal transduction, neuropathology, imaging, and radioresistance. Neoplasia (New York, N.Y.), 12(9), 675–684. https://doi.org/10.1593/neo.10688
- Zhang, Y., Dube, C., Gibert, M., Jr, Cruickshanks, N., Wang, B., Coughlan, M., Yang, Y., Setiady, I., Deveau, C., Saoud, K., Grello, C., Oxford, M., Yuan, F., & Abounader, R. (2018). The p53 Pathway in Glioblastoma. Cancers, 10(9), 297. https://doi.org/10.3390/cancers10090297
- Liu, A., Hou, C., Chen, H., Zong, X., & Zong, P. (2016). Genetics and Epigenetics of Glioblastoma: Applications and Overall Incidence of IDH1 Mutation. Frontiers in oncology, 6, 16. https://doi.org/10.3389/fonc.2016.00016
- Haider AS, Ene CI, Palmisciano P, Haider M, Rao G, Ballester LY and Fuller GN (2023) Concurrent IDH1 and IDH2 mutations in glioblastoma: A case report. Front. Oncol. 13:1071792. doi: 10.3389/fonc.2023.1071792
- Kanderi T, Munakomi S, Gupta V. Glioblastoma Multiforme. [Updated 2024 May 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558954/
- Lo H. W. (2010). EGFR-targeted therapy in malignant glioma: novel aspects and mechanisms of drug resistance. Current molecular pharmacology, 3(1), 37–52. https://doi.org/10.2174/1874467211003010037
- Singh, N., Miner, A., Hennis, L., & Mittal, S. (2021). Mechanisms of temozolomide resistance in glioblastoma – a comprehensive review. Cancer drug resistance (Alhambra, Calif.), 4(1), 17–43. https://doi.org/10.20517/cdr.2020.79